ihumaxn
16 June 2025
No Comments
Uncategorised
Don Payne
72 y/o
5′ 10″ (178 cm)
180.0 lb (81.8 kg)
Reason for encounter
Difficulty swallowing
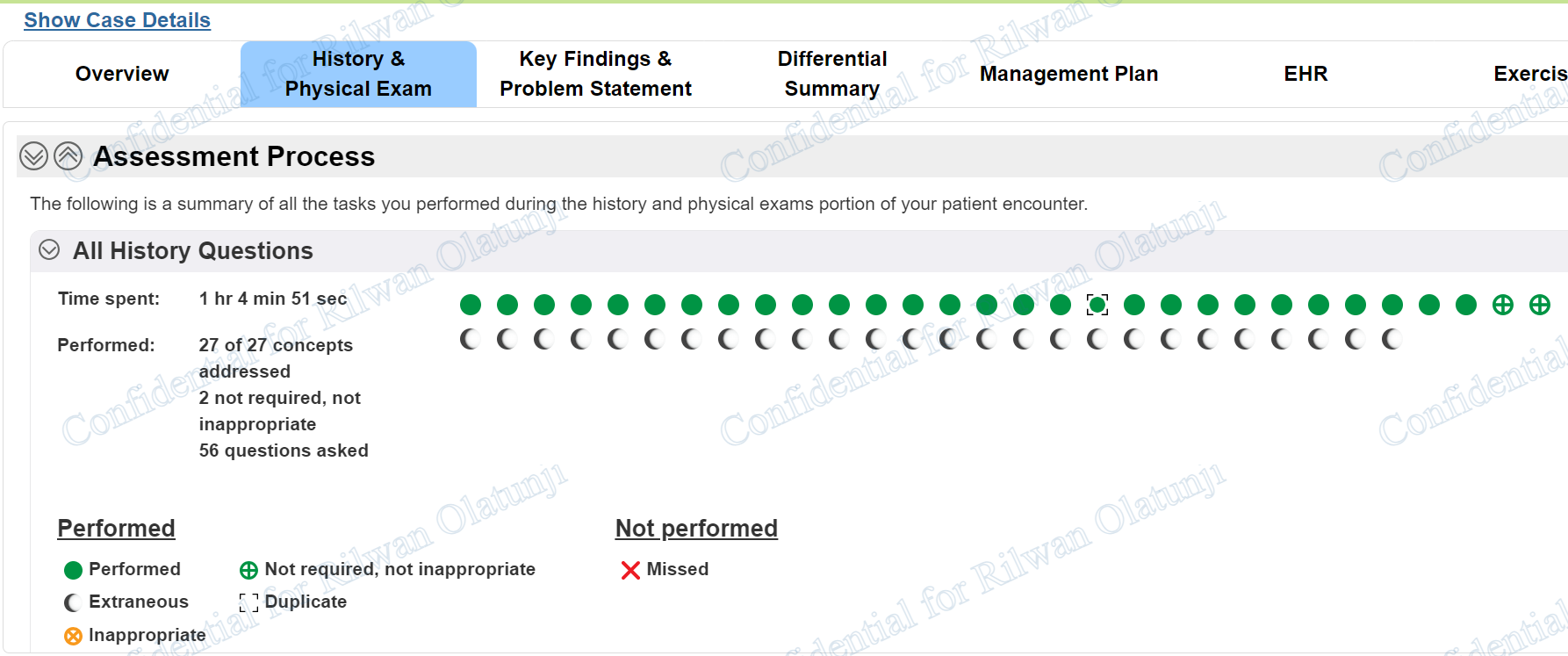
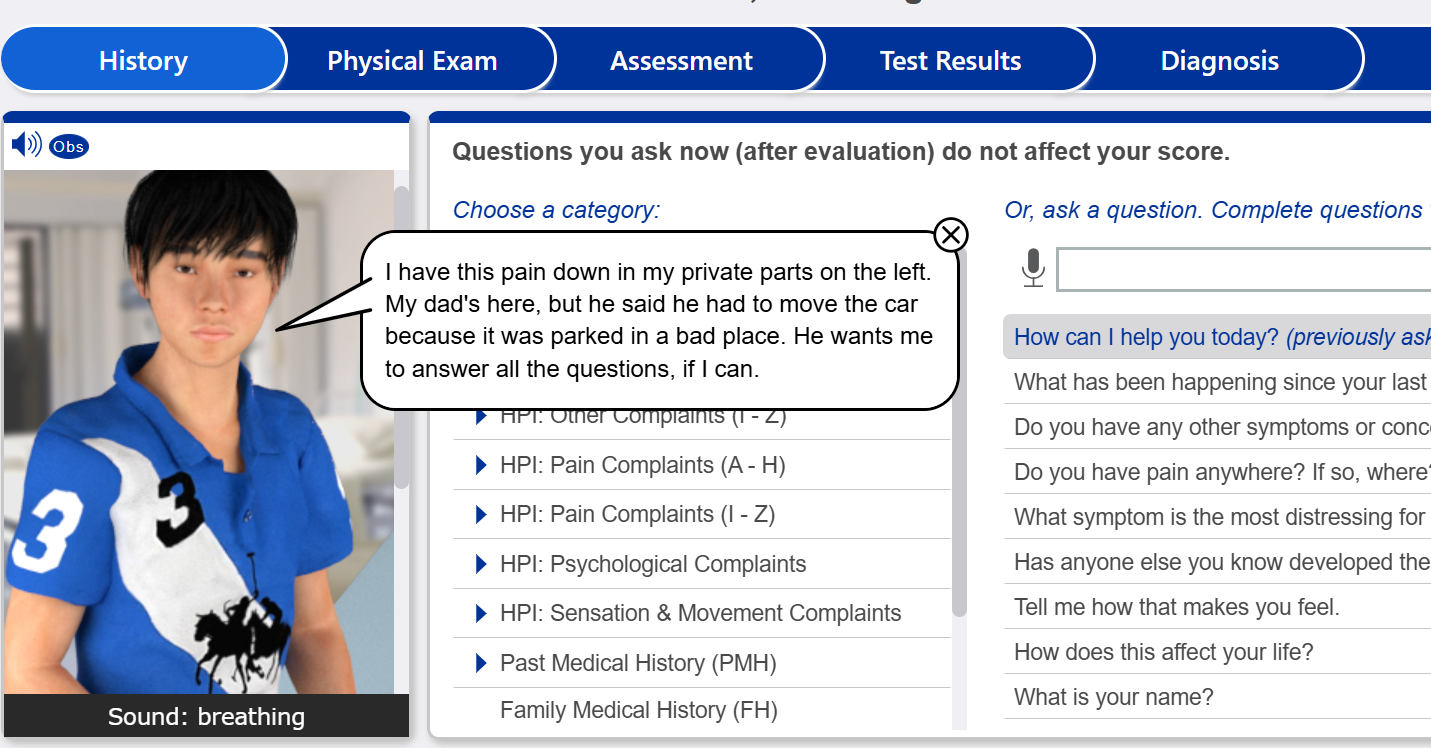
Interview History Questions
- What is your name?
- How can I help you today?
- Do you have any other symptoms or concerns we should discuss?
- Do you have pain anywhere? If so, where?
- What symptom is the most distressing for you?
- Tell me how that makes you feel.
- How does this affect your life?
- Have you gained or lost weight unintentionally, despite normal appetite and exercise?
- Do you have a cough
- Do you have any other symptoms or concerns we should discuss
- ………….
Physical Exams Required
- Weight
- Height
- cognitive status
- SpO2
- temperature
- blood pressure
- pulse
- respiration
- temperature
- auscultate heart
- auscultate lungs…….