ihumaxn
14 November 2024
No Comments
Uncategorised
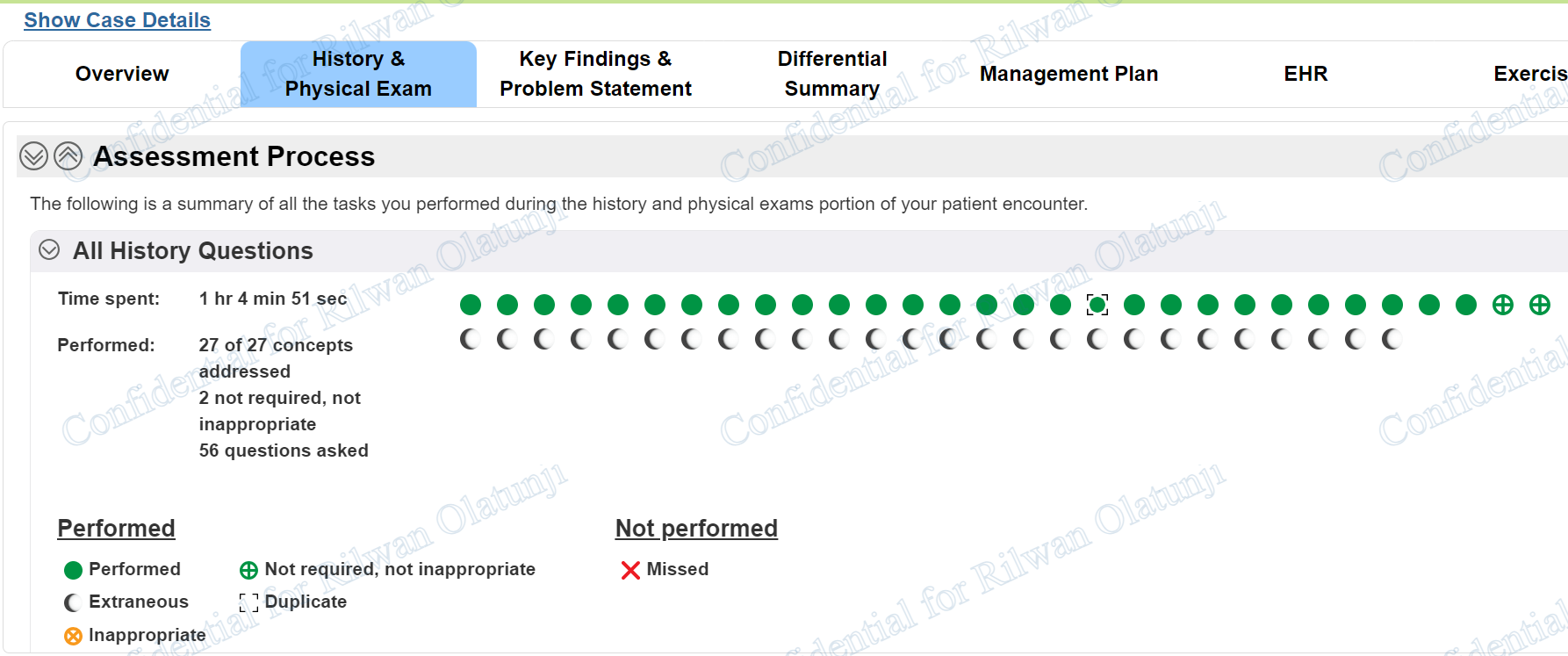
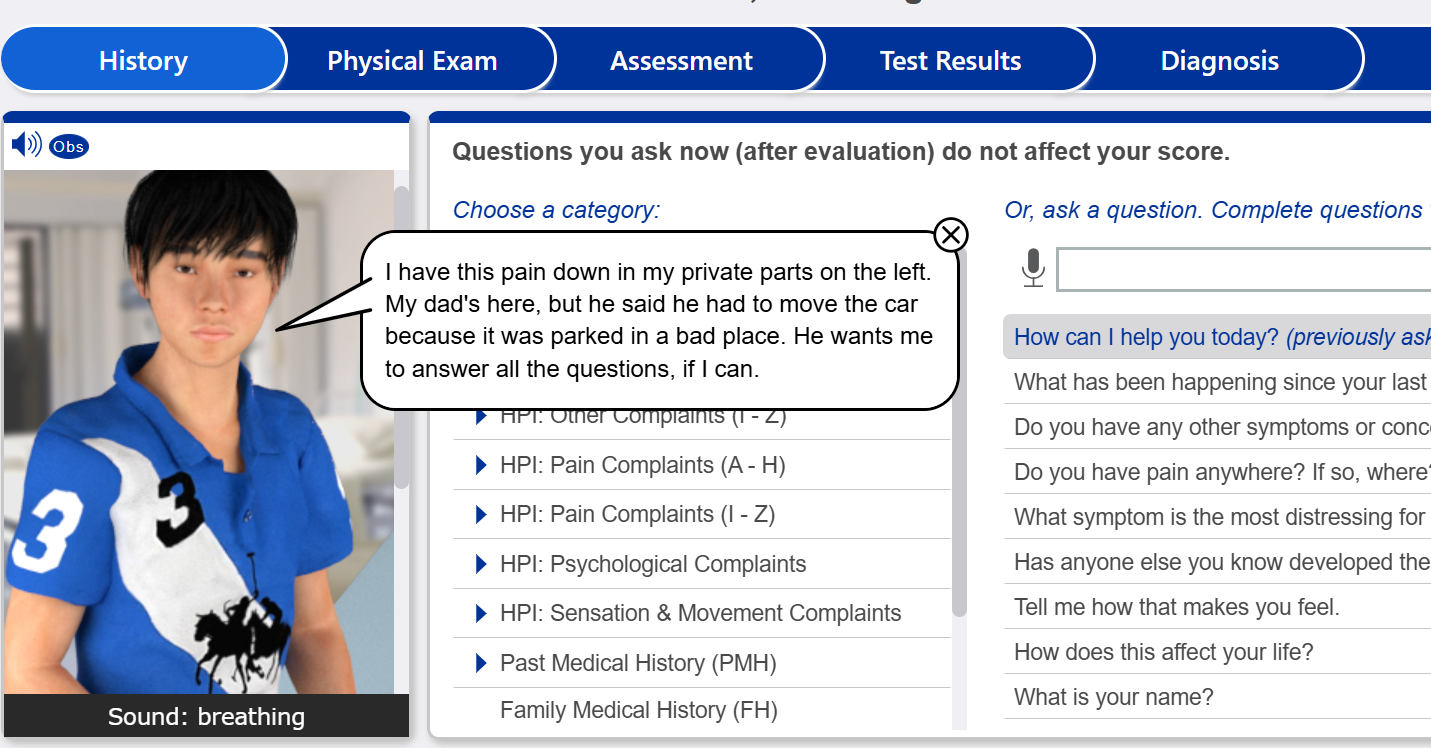
i-Human Case Week #10
13 y/o
5′ 5″ (165 cm)
120.0 lb (54.5 kg)
Reason for encounter
testicular pain
Case Problem Statement
The patient is a 13-year-old male who experienced the sudden onset of pain in the left scrotum during physical activity 2 hours prior to ED presentation. He has associated nausea, and has vomited once since the onset of pain. He has had no similar prior occurrences. On physical exam he appears to be in significant pain and is restless. He is tachycardic and diaphoretic, yet afebrile. Genital exam reveals left scrotal tenderness, swelling, and redness, with an absent cremasteric reflex ipsilaterally.
I-HUMAN PATIENTS CASE STUDY: ASSESSING THE GENITOURINARY AND REPRODUCTIVE SYSTEMS
Patients are frequently uncomfortable discussing with healthcare professionals issues that involve the genitalia and rectum; however, gathering an adequate history and properly conducting a physical exam are vital. Examining case studies can help prepare advanced practice nurses to accurately assess patients with problems in these areas.
For this i-Human Patients Case Study Assignment, you will examine and work with a patient with a condition of the genitourinary and/or reproductive system.
Click here to get the History Questions to ask for this iHuman Case. No payment upfront, only pay after you are satisfied with your grade.
Review of Systems
General patient denies sore throat, fevers, weight loss/weight gain, changes in appetite,
night sweats or chills.
Integumentary / Breast
HEENT / Neck denies trauma to head, dizziness, headache, vision loss, abnormal ear discharge, ear
pain, pain/difficulty swallowing, hoarseness, loss of smell, or nasal discharge. Denies
neck swelling/masses, with neck movement, swelling or lumps in neck (back or
front) or pain with moving the neck.
Cardiovascular patient denies palpitations, history of murmurs, chest pain/discomfort.
Respiratory patient denies exposure to secondhand smoke, denies cough, shortness of breath
(SOB), wheezing, or difficulty breathing.
Gastrointestinal
Genitourinary
Musculoskeletal patient reports genital pain with movement/walking, denies joint pain/stiffness,
muscle pain/swelling, or swelling in extremities, trunk, or neck.
Allergic / Immunologic patient denies known/unknown allergies to environment, food, or medication.
Endocrine patient denies changes in appetite, increased thirst/urination, weight gain/weight
loss, excess hair growth/loss on arms, face, or legs.
Hematologic / Lymphatic patient denies lack of energy, anemia (self or familial history), blue or cold hands,
lips, or feet, spontaneous bleeding or bruising.
Neurologic denies stroke like symptoms, loss of consciousness, headaches, fainting, loss of
memory, or dizziness.
Psychiatric patient denies thoughts of wanting to physically inflict harm to self/others, denies
anxiety, depression, hallucinations auditory or visual, homicidal/suicidal ideations.